Abstract

Introduction: Despite the large body of research in cancer and increasing numbers of cancer survivors, knowledge about the risks and prognoses related to thrombocytopenia in the clinical care setting is scarce. Such information is important to understanding the need and potential impact of platelet transfusion and emerging drug therapies for thrombocytopenia. In this study, we examined the risk of thrombocytopenia among patients with incident cancer. Further, we studied the extent to which thrombocytopenia was associated with adverse clinical outcomes.
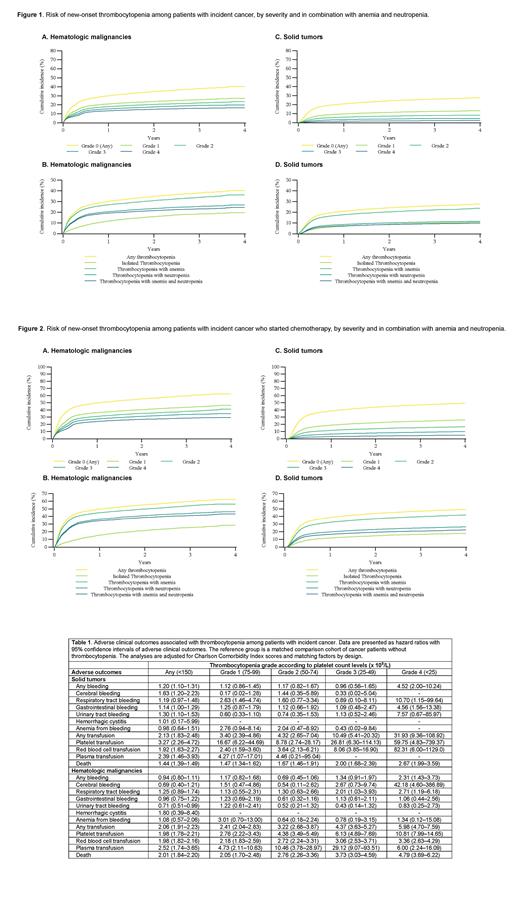
Methods: This population-based cohort study was conducted using data from the Danish Cancer Registry. All patients diagnosed with incident hematologic malignancies and solid tumors (age of ≥18 years) during 2015─2018 were identified. Data were linked with routine laboratory test results from the primary care and hospital settings, as recorded in the Danish Register of Laboratory Results for Research. Based on platelet count levels (x 10 9/L), thrombocytopenia was categorized as grade 0 (any count)<150; grade 1:<100; grade 2:<75; grade 3:<50; and grade 4: <25. We tabulated the prevalence of thrombocytopenia at study inclusion and calculated the cumulative incidence proportion (risk) of thrombocytopenia, accounting for the competing risk of death. Each patient with thrombocytopenia was matched up to 5 cancer patients without thrombocytopenia by age, sex, cancer type, cancer stage, and time from cancer diagnosis and index date. Cox proportional hazards regression analysis was used to compute hazard ratios (HRs) with 95% confidence intervals (CIs) of adverse clinical outcomes, including any bleeding leading to hospitalization, site-specific bleeding leading to hospitalization, transfusion (red blood cell, platelet, or fresh frozen plasma), and death. HRs were adjusted for Charlson Comorbidity Index scores and matching factors by design.
Results: The analytic cohort comprised 11,785 patients with hematologic malignancies and 57,600 patients with solid tumors (median age=70 years). Any thrombocytopenia was observed during the 6 months preceding study inclusion among 18% of patients with hematologic malignancies (grades 1-2: 6% and grades 3-4: 5%) and 4% of patients with solid tumors (grades 1-2: 1% and grades 3-4: 0%). The 1-year and 4-year risks of new-onset thrombocytopenia were 30% and 40% for hematologic malignancies and 21% and 28% for solid tumors, respectively (Figure 1). Among patients who initiated chemotherapy following their cancer diagnosis (n=33,165), the 1-year and 4-year risks of thrombocytopenia were 50% and 62% for hematologic malignancies and 39% and 49% for solid tumors, respectively (Figure 2). Patients with grade 4 thrombocytopenia had higher rates of any bleeding leading to hospitalization than patients without thrombocytopenia [hematologic malignancies: HR=2.31 (95% CI: 1.43-3.73) and solid tumors: HR=4.52 (95% CI: 2.00-10.24)], while grades 1-3 thrombocytopenia did not confer a significantly increased rate of hospitalization for bleeding (Table 1). All grades of thrombocytopenia were associated with an increased rate of transfusion [overall for hematologic malignancies: HR=2.06 (95% CI: 1.91-2.23), and overall for solid tumors: HR=2.13 (95% CI: 1.83-2.48)] and with death [overall for hematologic malignancies: HR=2.01 (95% CI: 1.84-2.20), and overall for solid tumors: HR=1.44 (95% CI: 1.39-1.49)]. These associations increased in magnitude with decreasing platelet count levels.
Conclusions: The risk of thrombocytopenia was substantial following a diagnosis of incident hematologic malignancy and solid tumors, with higher risks among patients who initiated chemotherapy. While only severe thrombocytopenia was a predictor of any hospitalization for bleeding, all grades of thrombocytopenia were associated with increased rates of transfusion and death. Our findings support the need for regular assessment of platelet count levels to identify cancer patients at risk of serious clinical outcomes.
Clouser: Amgen: Current Employment, Other: This work is related to Chemotherapy Induced Thrombocytopenia as a disease state, in this essence it is not directly related to an Amgen product; CIT is an area of scientific interest to Amgen with Romiplostim under development for this potential indicati. Saad: Amgen: Current Employment, Current equity holder in publicly-traded company.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal